
OFFICE HOURS |
OFFICE INFORMATION |
||
|
Monday - Friday |
8:30am - 4:30pm |
980 Westfall Road |
[Phone] 585.442.1110 |
I Would Like To:
|
Hoarseness & Voice Changes
C. Michael Haben, M.D., M.Sc. Rochester, NY
Abstract: This treatise on hoarseness is intended for primary care physicians and mid-level providers. It is produced by the Center for the Care of the Professional Voice, part of the Haben Practice for Voice & Laryngeal Laser Surgery, PLLC, specializing in voice disorders and laryngology in Rochester, NY. It provides a comprehensive listing of common voice disorders, key elements of the patient's history, findings at laryngoscopy and recommendations for specialist referral.
Key Words: Hoarse, voice, larynx, polyp, cancer, paralysis, papilloma, laryngitis.
History: there are many important features of a patient's history to consider when presented with a voice change. Although an exhaustive list is beyond the scope of this text, some key considerations include the patient's professional and social vocal obligations. Individuals employed in a loud call center, or work in sales; or those with history of voice overuse/ abuse (i.e. cheerleading, outdoor team sports, yelling) have a predilection for certain voice problems. A drastic increase or cessation of voice use is also important to consider. A classic "underuse" example is that of an elderly person with the death of a spouse who now lives alone. Singers are a special class of voice user who tend to present with subtle voice changes early on and involving only the singing voice, without abnormalities in speaking voice quality. A "singing voice history" is very specialized, necessitating an early referral. Personality is certainly a factor. Loud or talkative personality tends to predict chronic voice overuse and predisposes to nodules, polyps and scarring of the vocal folds. Significant improvement of a voice problem with voice rest tends to indicate a functional problem, whereas minimal variability with voice usage may indicate a fixed lesion. Any condition which affects the respiratory system, such as recent (prolonged) hospitalization, asthma exacerbation or allergies, affects the voice. The lungs are the "power supply" of the voice, and are, in part, responsible for the "old voice" in many elderly persons. Neurologic co-morbidities and family history may play a role in vocal tremors. Current or prior tobacco and alcohol consumption is important, as is a history of gastroesophageal reflux disease. Each of these are risk factors for malignancy. Inhaled medications, especially corticosteroids, may impact voice quality directly or indirectly, via precipitation of laryngeal candidasis. The acuteness of the voice change and antecedent events such as surgery or viral illnesses are critical factors. Postoperative voice changes may be the result of endotracheal intubation or surgical trauma, especially in long procedures or those which involve the neck or chest region by putting the recurrent laryngeal nerves at risk. "Hyper-acute" atraumatic instantaneous voice loss is frequently seen with malingering. Secondary gain can sometimes be discovered. Finally, many psychiatric disorders manifest as voice changes, from weakness seen in depression, to complete aphonia. A careful history can usually provide clues as to the nature of the voice problem, and is critical in identifying lifestyle or behavioral components which are part of the long term management. Direct laryngoscopy with vocal capability battery, however, is the gold standard for most laryngeal conditions and only rarely can an accurate diagnosis be made on the basis of history alone. The timing for referral for direct laryngoscopy and voice evaluation will vary greatly depending upon the clinical situation. Guidelines for referral will be addressed for each of the common conditions considered here.
Character: hoarseness is a symptom and not a diagnosis. Patients may describe a variety of voice disturbances as being "hoarse", "raspy" or "laryngitis." Characterizing the voice change can provide important information in establishing a diagnosis and is the first step of a "vocal capability battery." For example, a very breathy voice could indicate a paralyzed vocal fold. Additionally, a weak monotonous quality could indicate a neurologic condition such as Parkinson's Disease. Voice quality is best characterized as being predominantly hoarse, rough, breathy, weak, tremulous, and abnormally low/high pitched. Descriptive voice terminology will be italicized for each condition presented.
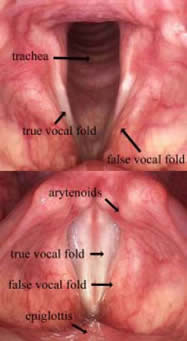 Laryngoscopy: all images in this manuscript were acquired in the clinic and are orientated in a manner as if they were being viewed by indirect laryngoscopy (mirror examination) with the bottom of each image being anterior. For some conditions, indirect laryngoscopy performed by capable practitioners, in conjunction with an appropriate history could establish an accurate diagnosis. As a technique, indirect laryngoscopy requires practice. Not simply just to perform the examination, but to become proficient in identifying normal and abnormal anatomy. The normal laryngeal anatomy is highlighted with the glottis closed, as during respiration (top image), and open, as during phonation (bottom image). Relevant structures are labeled. Normal vocal folds are pearly white due to a paucity of lymphatics or extensive vasculature in the superficial layers. The vocal folds open and close symmetrically, and although the two sides are more or less mirror images, asymmetry is not uncommon. The vibratory medial edges are straight and close completely during phonation. In some individuals, the subglottis and proximal trachea can be visualized. Some or all of these structures can be identified in most individuals via mirror examination. An inability to adequately visualize the larynx is a strong indication for specialty referral.
Laryngoscopy: all images in this manuscript were acquired in the clinic and are orientated in a manner as if they were being viewed by indirect laryngoscopy (mirror examination) with the bottom of each image being anterior. For some conditions, indirect laryngoscopy performed by capable practitioners, in conjunction with an appropriate history could establish an accurate diagnosis. As a technique, indirect laryngoscopy requires practice. Not simply just to perform the examination, but to become proficient in identifying normal and abnormal anatomy. The normal laryngeal anatomy is highlighted with the glottis closed, as during respiration (top image), and open, as during phonation (bottom image). Relevant structures are labeled. Normal vocal folds are pearly white due to a paucity of lymphatics or extensive vasculature in the superficial layers. The vocal folds open and close symmetrically, and although the two sides are more or less mirror images, asymmetry is not uncommon. The vibratory medial edges are straight and close completely during phonation. In some individuals, the subglottis and proximal trachea can be visualized. Some or all of these structures can be identified in most individuals via mirror examination. An inability to adequately visualize the larynx is a strong indication for specialty referral.
Common Voice Conditions
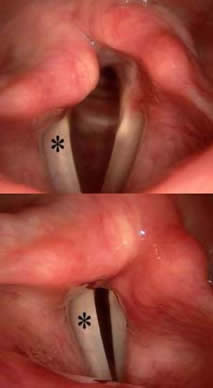 Diagnosis: right * vocal fold paralysis
Diagnosis: right * vocal fold paralysis
History: almost invariably an acute onset change in voice is elicited, sometimes with a history of an antecedent viral URI. May also occur post-operatively, especially following cervical or thoracic surgery where the recurrent laryngeal nerves are at risk. The voice change is noted abruptly upon extubation. In true idiopathic or post-viral cases, patients commonly awaken with a changed voice, or find it has deteriorated over a period of hours. The voice is best described as being a breathy dysphonia with an abnormally high-pitched "Mickey Mouse" quality. Complaints of a weak cough and dysphagia are not uncommon.
Laryngoscopy: the immobile (right *) side is in a fixed position when modulating between respiration (top image) and phonation (bottom image) with an inability to fully close the glottis and engage the vibratory edges. There will always be a degree of internal rotation of the larynx which is best appreciated posteriorly. Pooled secretions may be seen posteriorly (hypopharynx).
Referral: semi-urgent consultation for confirmatory direct laryngoscopy should be done in all cases. Direct laryngoscopy is diagnostic of the vocal fold immobility, however, further work-up is frequently necessary. In presumed post-viral and idiopathic cases, a CT scan of the length of the recurrent laryngeal nerve is mandatory to exclude benign or malignant neoplasms which may be impinging upon, or invading, the recurrent laryngeal nerve. This may occur anywhere along the nerve's course, from the intracranial / skull base segment (i.e. meningioma); cervical region (i.e. laryngeal, esophageal or thyroid malignancy); and the chest (i.e. metastatic cancer). Imaging is not indicated in many post-operative cases.
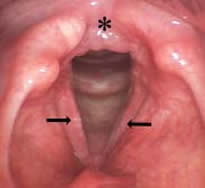
 Diagnosis: larynx cancer: CIS/ carcinoma-in-situ (top image), T1 (early) laryngeal
carcinoma (middle image), T3 (advanced) laryngeal carcinoma (bottom image)
Diagnosis: larynx cancer: CIS/ carcinoma-in-situ (top image), T1 (early) laryngeal
carcinoma (middle image), T3 (advanced) laryngeal carcinoma (bottom image)
History: 98% of persons diagnosed with laryngeal cancer have a present or former
smoking history. Rarely, it is diagnosed in lifetime non-cigarette smokers. These
persons tend to have a history of extensive second-hand smoke exposure, severe
gastroesophageal reflux disease, prior laryngeal papillomatosis (HPV) or non
cigarette smoking (i.e. cigars, marijuana). Although the amount and duration of
smoking is important (e.g. pack/years), as is the length of time since smoking
cessation, a high index of suspicion should be maintained in all current or former
tobacco consumers who present with voice changes. Voice changes tend to be
subacute in onset and progressive in severity. The character of the voice varies
from mild- moderate hoarseness, to complete aphonia, that varies minimally with
voice rest or extent of voice usage.. The size of the tumor, proximity and inhibition
of engagement of the vibratory edges will dictate the degree of hoarseness.
Laryngoscopy: pre-cancer and cancer of the vocal folds can vary widely in appearance from flat white keratotic patches, deeply ulcerative lesions, or large obstructing exophytic masses. Carcinoma forms on the vocal folds in 80-90% of all larynx cancer cases, and typically presents as hoarseness. By contrast, supraglottic lesions, represent <10% of larynx cancer, and tend to be asymptomatic early and usually present as dysphagia or a neck mass when they grow to an advanced stage. Carcinoma is one of only two common disease processes to involve the vocal fold epithelial cover (papillomatosis, being the other). The degree of spread along the epithelial covering determines early stage (I & II) laryngeal cancer, with mobility of the vocal fold and deep spread determining advanced stages (III & IV).
Referral: laryngoscopy is indicated in all cases of hoarseness in "at risk" individuals whose unexplained voice change persists for more than 2 weeks or when a highly reliable mirror examination can not be performed. Once a suspicious lesion is identified, work-up will begin with tissue biopsy, and staging imaging in most patients. Synchronous second malignancies can occur in up to 20% of laryngeal cancer patients.
 Diagnosis: presbyphonia (vocal fold atrophy)
Diagnosis: presbyphonia (vocal fold atrophy)
History: usually insidious onset voice changes, which may be acute after a life event, such as the death of a spouse or prolonged hospitalization, especially if intubated. This is due to deconditioning and relative disuse of the voice, exacerbated by a notable decrease in pulmonary function following prolonged illness or hospitalization. Patients generally are septogenarians & octogenarians. The voice frequently has a weak "old person" quality, with or without a notable tremor or roughness. Patients complain that the voice worsens with extended usage (> 10 minutes) or in social situations (i.e. "I can't be heard across the table"). Interestingly, the person's voice may sound normal for gender and age, and the real issue in social situations lies with the hearing status of the patient's peers.
Laryngoscopy: atrophic appearing vocal folds with thinning of the vibratory edges. Asymmetries in appearance and movement are not uncommon. Commonly referred to as "vocal fold bowing."
Referral: usually necessary to exclude malignancy, or in those whom may benefit from targeted speech therapy.
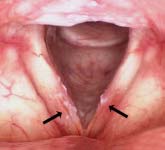
 Diagnosis: reflux laryngitis
Diagnosis: reflux laryngitis
History: there is typically mild to moderate hoarseness with subacute onset. These are frequently associated with other chronic throat symptoms including cough,
throat clearing, globus, discomfort and excessive phlegm. There may or may not be a history of heartburn, and its absence does not exclude reflux laryngitis.
Behavioral habits may be positive for tobacco, alcohol, carbonated beverages,
excessive coffee/ caffeine intake, high stress lifestyle or late meals.
Laryngoscopy: hyperemia of vocal fold epithelium with edema in the interarytenoid region (*) are some of the myriad findings. Thickened endolaryngeal mucus is also common (seen anteriorly), as is pooling of clear secretions in the hypopharynx. The severity of laryngeal findings does not often correspond to the severity of the patient's symptoms.
Referral: reflux disease is an independent risk factor for carcinoma of the upper aerodigestive tract, especially
esophageal. A trial of empiric acid suppression therapy with lifestyle modifications is reasonable in low-risk patients
with a positive history, however, direct laryngoscopy is indicated in high-risk individuals, or those failing a PPI trial.
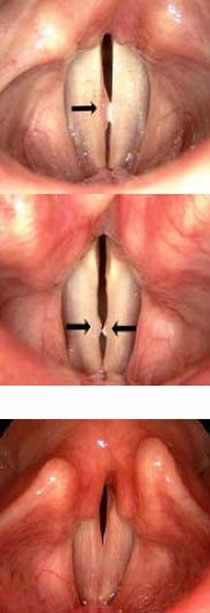 Diagnosis: vocal fold polyp/ nodules
Diagnosis: vocal fold polyp/ nodules
History: patient complains of subacute to insidious onset, protracted "laryngitis." Usually a history of significant vocal obligations / voice overuse (i.e. bartending, aerobics instructor) is elicited. The overuse is usually chronic. The severity of the hoarseness tends to fluctuate with voice usage, without fully returning to normal. Speaking voice will have a hoarse character, with the degree depending upon the size of the lesion. Polyps are less associated with excessive vocal trauma than nodules, and a negative history of voice abuse is infrequently obtained.
Laryngoscopy: polyps & nodules are along a continuum of changes that occur along the vibratory margin of one or both vocal folds. The upper image is of a polyp of the right vocal fold. The lower image is that of nodules, bilaterally. By definition, they are not growths, and are analogous to a callus or a boil.
Referral: direct laryngoscopy is indicated in cases that fail conservative measures, necessitate confirmation or in all professional voice users. Strict voice rest is only indicated as a short-term, temporary solution, analogous in long term efficacy to a "crash diet." Speech therapy should be considered only after diagnosis is confirmed by laryngoscopy.
Diagnosis: acute laryngitis
History: acute onset voice change with an antecedent or concurrent viral upper respiratory tract infection. In cases where a antecedent viral prodrome is not elicited, a current exacerbation of pre-existing seasonal or environmental allergies may be found. Generally, no ameliorating or exacerbating factors are identified. The is moderate to moderately-severe hoarseness that may last for weeks.
Laryngoscopy: generalized hyperemia of vocal fold epithelium with edema of the superficial layers giving the appearance of "swollen cords."
Referral: generally reserved for cases of presumed acute viral laryngitis that fail to resolve with conservative measures or within a reasonable time frame.
 Diagnosis: recurrent respiratory papillomatosis (HPV)
Diagnosis: recurrent respiratory papillomatosis (HPV)
History: initial presentation is that of slowly progressive voice changes over a period of months, or even years. The features and progressive nature of the loss of voice is similar to laryngeal carcinoma, yet, a significantly younger age at presentation and lack of risk factors are the norm. Papillomas of areas of the larynx not involved with vibration and phonation are generally asymptomatic. Papillomatosis may initially present in any age group, however, a bimodal distribution is seen at 7-13 and 20-40 years of age. A hoarse voice will be the only symptom in most cases, with minimal variability related to voice usage. The severity of the hoarseness is dictated by the burden of disease involving the vibratory tissues. A history of prior papillomatosis as a child (juvenile onset RRP) should strongly raise suspicion for adult recurrence. Serology is of no diagnostic value.
Laryngoscopy: papillomas, like carcinoma, are epithelial diseases. They are caused by human papilloma virus (HPV) infection and may be unifocal, multi-focal, or "carpeting" the entire laryngeal surface. Classic papillomas appear like a "bunch of grapes" with red dots (circled), that are actually spiral capillary ectasias. Some papillomas are dysplastic, or even harbor malignancy, and have a keratotic appearance somewhere between classic papilloma and malignancy.
Referral: direct laryngoscopy, biopsy and viral typing is indicated in all new patients suspected of having laryngeal papillomatosis. Due to the recalictrant and relapsing nature of laryngeal papillomas, and the risk for malignant degeneration, patients should be routinely followed by a qualified laryngeal surgeon.
 Diagnosis: benign smoker's polyp
Diagnosis: benign smoker's polyp
History: insidious onset voice changes seen almost exclusively in women, whose voice is often confused with a man's over the telephone. Talkative personality is common, and smoking history is generally of 20 years duration or more. Shortness of breath may be present if the polyp is obstructing. The voice is best described as being both hoarse and low-pitched for gender.
Laryngoscopy: obstructing (*) pedunculated "fluid filled sac" with intact
epithelium. In this example: "ball-valving" into the airway with respiration.
Referral: the initial diagnosis of smoker's polyps is impossible to distinguish from malignancy on clinical grounds, even with a well-documented mirror examination. Early specialty referral is mandatory.
 Diagnosis: malingering
Diagnosis: malingering
History: "hyper-acute" atraumatic near-complete voice loss that can happen in an instant. One may also awaken with "a squeak" for a voice without an identifiable antecedent event. Secondary gain may or may not be readily discoverable. Paradoxical softening of the voice is noted when patient is asked to shout or yell. A hallmark feature is a loud, strong, unaffected cough. Malingering may be clinically difficult to differentiate from psychogenic voice disorders. The voice is classically excessively high-pitched or voiceless mouthing of words.
Laryngoscopy: normal laryngeal anatomy and movement. Certain maneuvers can be accomplished during direct laryngoscopy to confirm the diagnosis, however are difficult to achieve using a mirror.
Referral: early specialist referral recommended. A trial of speech therapy prior to a confirmatory diagnosis tends to prolong and reinforce the underlying problem rather than help in achieving or regaining voice.
 Diagnosis: muscle tension dysphonia
Diagnosis: muscle tension dysphonia
History: far more common in men, 60 years of age or older. Insidious onset voice changes not infrequently associated with throat discomfort while using the voice. Voice can vary from day to day, or within the same day. Vocal quality is typically worse when projected, later in the day, social situations or when used for extended periods of time. Volitional cough is normal. The quality is best described as rough.
Laryngoscopy: engagement of the false vocal folds (*) during phonation which dampens true vocal fold vibration. Supraglottic hyper-function is thought to be compensatory for glottic insufficiency due to presbyphonia / age.
Referral: direct laryngoscopy is confirmatory. It is a very difficult diagnosis to establish and to visualize the true vocal folds to exclude malignancy using a mirror. A trial of speech therapy is reasonable once the diagnosis is confirmed.
 Diagnosis: laryngeal candidiasis
Diagnosis: laryngeal candidiasis
History: in the larynx, occurs exclusively in persons using inhaled steroids, in
contrast to oropharyngeal thrush where oral antibiotic and certain co-morbidities
can precitipate fungal overgrowth. Voice changes tend to be progressive over
several days and characterized by moderately-severe persisting hoarseness that
varies little from day to day or with voice usage. Odynophagia is not uncommon.
Laryngoscopy: hyperemia of the vocal folds with gross fungal colonies (arrows) are easily visualized and diagnostic without the need for cultures in most cases.
Referral: direct laryngoscopy is considered the gold standard, however, a quality mirror examination can often be diagnostic. Keratosis and candida have a similar appearence. A positive history for inhaled steroid use is very important.
 Diagnosis: vocal fold hemorrhage
Diagnosis: vocal fold hemorrhage
History: severe acute onset loss of voice following a period of significant voice overuse/ abuse, such as yelling during an argument or shouting at a sporting event. Rarely, this can occur in a professionally trained singer who hits a note "just right" and suddenly losses the voice. Character is usually severe hoarseness or even complete aphonia that slowly improves over 1-2 weeks.
Laryngoscopy: hemorrhage under the epithelium of one or both vocal folds.
Referral: indicated in professional voice users, lack of complete resolution after 2 weeks, or atypical history (i.e. presence of hemoptysis, no history of voice abuse).
The author would like to acknowledge the contributions of Dr. Geoffrey Morris, Pulsifer Medical Associates, Rochester, NY.